Clair, A. et al, 24 May 2016, The impact of housing payment problems on health status during economic recession: A comparative analysis of longitudinal EU SILC data of 27 European states, 2008–2010, excerpt:
Showing posts with label health. Show all posts
Showing posts with label health. Show all posts
Monday 10 December 2018
Australia 2018: Is long-term rental destroying the wellbeing of low income households?
Across the nation,
people who rent are living on insecure tenancies. Almost 9 in 10 Australians
who rent (88%) are on leases of a year or less, and are not certain of where
they will be living in a year’s time. This impacts a person’s ability to feel
part of the local community and establish roots.
The
Land, 1 May
2018:
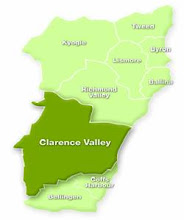
AFFORDABLE rentals on
the state’s North Coast are increasingly few and far between, but the
continued rise of the Airbnb-model now sees 3000-plus homes sit empty
while low-income and government-assisted tenants are shut out.
Anglicare’s latest
Housing Affordability Snapshot says the region’s rental crisis has
worsened as property owners in Ballina, Byron Bay, and the Tweed are
incentivised to target short-term holidaymakers through web-based booking
companies instead of potential long-term renters.
The Anglicare report,
released on Sunday, showed available
North Coast rental properties were in steep decline (down from 795 in
2017 to 660 in 2018) with all family groups on income support, and single
households on minimum wage, likely to struggle to find housing for themselves
and their children.
Clair, A. et al, 24 May 2016, The impact of housing payment problems on health status during economic recession: A comparative analysis of longitudinal EU SILC data of 27 European states, 2008–2010, excerpt:
Transitioning into
housing arrears was associated with a significant deterioration in the health
of renters…..
Housing arrears is one
of the so-called ‘soft’ ways in which housing influences health (Shaw, 2004),
especially mental health, alongside the ‘hard’, physical impacts of the
infrastructure itself, such as damp, mould, and cold. A growing body of
scholarship indicates that people who experience housing insecurity,
independent of other financial difficulties, experience declines in mental health
(Gili et al., 2012, Keene et al., 2015, Meltzer et al., 2013, Meltzer et al., 2011, Nettleton and Burrows, 1998).
In Australia, analysis of the longitudinal HILDA dataset found that those in
lower income households who had moved into unaffordable housing experienced a
worsening in mental health (Bentley, Baker, Mason,
Subramanian, & Kavanagh, 2011), with male renters faring worse (Bentley et al., 2012, Mason et al., 2013).
One has to
wonder if being a long-term renter affects quality of life to such a degree
that on average renters die earlier than
home-owners.
Labels:
Australian society,
cost of living,
health,
housing,
Northern Rivers
Friday 30 November 2018
Call to protect infants from dangerous infectious disease, whooping cough
The Daily Examiner, 27 November 2018, p3:
NSW Health is urging all
pregnant women and new parents to be aware of the symptoms of whooping cough
and to ensure they and their children are vaccinated on time.
Despite almost 95 per
cent of infants in NSW now vaccinated against the disease, outbreaks still
occur every three to four years as community immunity wanes, and recent high
numbers indicate an outbreak might be on the way.
Dr Vicky Sheppeard, NSW
Health’s Director of Communicable Diseases, said that in October 2018 almost
800 people in NSW were notified with whooping cough (pertussis), the highest
number since October 2016.
Acting director of North
Coast Public Health Greg Bell said a similar situation was emerging in Northern
NSW where there have been 36 cases of whooping cough reported in the past four
weeks.
While these levels of
whooping cough across Northern NSW are similar to the averages of the previous
five years, pertussis notifications are trending upwards.
The latest Australian
Immunisation Register quarterly report shows that at September 2018 90.4 per
cent of five-year-olds and 88.9 per cent of 12-month-olds in Northern NSW Local
Health District were fully vaccinated.
These figures represent
an increase on vaccination rates in 2010 under the-then North Coast Area Health
Service, when 84.9 per cent of children aged 5 and 87 per cent of 12-month-olds
were fully vaccinated.
Even in highly
vaccinated populations it is not possible to eliminate whooping cough…..
“The aim of whooping cough control is to
protect infants, who are at highest risk of severe disease or death if they
contract whooping cough. Whooping cough vaccination is effective in preventing
severe infection.”
Labels:
children,
disease outbreak,
health,
New South Wales
Friday 16 November 2018
Yet other digital privacy betrayals
The global situation......
The
Guardian, 14
November 2018:
Google has been accused
of breaking promises to patients, after the company announced it would be
moving a healthcare-focused subsidiary, DeepMind Health,
into the main arm of the organisation.
The restructure, critics
argue, breaks a pledge
DeepMind made when it started working with the NHS that “data will
never be connected to Google accounts or services”. The change has also
resulted in the dismantling of an independent review board, created to oversee
the company’s work with the healthcare sector, with Google arguing that the
board was too focused on Britain to provide effective oversight for a newly
global body.
“Our vision is for
Streams to now become an AI-powered assistant for nurses and doctors everywhere
– combining the best algorithms with intuitive design, all backed up by
rigorous evidence,” DeepMind said, announcing the
transfer. “The team working within Google, alongside brilliant colleagues
from across the organisation, will help make this vision a reality.”
DeepMind Health was
previously part of the AI-focused research group DeepMind, which is officially
a sibling to Google, with both divisions being owned by the organisation’s
holding company Alphabet.
But the transfer and
vision for Streams looks hard to reconcile with DeepMind’s previous comments
about the app. In July 2016, following criticism that the company’s
data-sharing agreement with the NHS was overly broad, co-founder Mustafa
Suleyman wrote:
“We’ve been clear from the outset that at no stage will patient data ever be
linked or associated with Google accounts, products or services.”
Now that Streams is a
Google product itself, that promise appears to have been broken, says privacy
researcher Julia Powles: “Making this about semantics is a sleight of hand.
DeepMind said it would never connect Streams with Google. The whole Streams app
is now a Google product. That is an atrocious breach of trust, for an already
beleaguered product.”......
Here in Australia......
Canberra Times, 15 November 2018, p.8:
The chairman of the
agency responsible for the bungled My Health Record rollout
has been privately advising a global healthcare outsourcing company. Fairfax
Media discovered the relationship between the UK-based company Serco and the
Australian Digital Health Agency (ADHA) chairman Jim Birch after
obtaining a number of internal documents.
The revelation comes
as Health Minister Greg Hunt was forced to extend the My Health Record opt-
out period after a compromise deal with the Senate crossbench and a last-minute
meltdown of the website left thousands of Australians struggling to meet the
original deadline.
Since April 2016, Mr Birch has been ADHA chairman with
oversight of My HealthRecord, the online summary of key health information
of millions of Australians. Documents from the ADHA, released under freedom of
information laws, show Mr Birch registered his work for Serco in November 2017,
but the relationship was never publicly declared.
After Fairfax Media
submitted questions last week on whether the relationship posed a conflict of
interest, Mr Birch quit the advisory role.
Serco has won a number
of multibillion-dollar government contracts to privately run - and in some
cases deliver healthcare in - some of Australia's prisons, hospitals and
detention centres.
The ability of Serco to
navigate the controversial area of digital health records would
be invaluable to any future expansion plans.
A spokeswoman for
federal Health Minister Greg Hunt said all board members had declared
their interests.
"Board members do
not have access to system operations, and board members cannot be present while
a matter is being considered at a board meeting in which the member has an
interest," she said.
Lisa Parker, a
public health ethics expert at University of Sydney, said the public
had been asked to trust the agency is acting in its best interests. She said
they should make public any information relevant to that trust…..
The register also shows
Mr Birch knows the chief executive of start-up Personify Care, Ken Saman, and
has been giving him advice since August last year. The software company
recently released "Personify Connect", a product that provides
hospitals with "seamless integration" of its original patient monitoring
platform with My Health Record.
Despite being scheduled
to speak at a "Personify Care breakfast seminar" later this year, Mr
Birch has never publicly declared this interest. Mr Birch is also chairman of
another start-up called Clevertar that allows businesses to create
"virtual agents" and offer "personalised healthcare support,
delivered at scale". This relationship is on the public record.
Public sector ethics expert Richard Mulgan, from Australian National
University, said the chairman should submit to a higher standard than ordinary
board members and distance himself from anything suggesting a conflict of
interest.
He said perception was
just as important as reality and the public, not the people involved, was the
best judge of whether there was a problem.
"The personal
interests register must be published," he said.
"The fact they
haven't can only lead to the perception there are conflicts of which they are
ashamed."
Mr Birch, Personify Care
and Clevertar did not respond to Fairfax Media's questions.
A Serco spokesman
confirmed the company met with Mr Birch "occasionally ... over the past 12
months regarding business management", but did not answer whether it paid
him.......
The Courier Mail, 15 November 2018, p.4:
Your dietitian, dentist,
podiatrist, occupational therapist or optometrist will be able to see if have a
sexually transmitted disease or an addiction unless you set access controls
to My Health Record.
Major new privacy
concerns emerged after the Federal Government was yesterday forced into an
embarrassing call to delay the rollout.
People trying to access
the controversial My Health Record hotline and computer
portal experienced major delays during a rush to opt out before the system was
rolled out tomorrow.
Health Minister
Greg Hunt was forced to delay the opt out period until January 31 after
pressure from health groups and crossbench senators.
The Australian Medical
Association was the only major health group not calling for a delay.
The vast majority of
groups were concerned the record would come into effect before key
privacy and security upgrades had been passed by Parliament. AMA president Dr
Tony Bartone denied its position was related to his need to keep the Health Minister
onside while he negotiated key reforms to general practice care.
Wednesday 24 October 2018
Morrison Liberal-Nationals Coalition Government begins to position itself for forthcoming federal election
No, the Morrison Coalition Government has not suddenly developed empathy for others, a genuine understanding of its obligations under international law or a measure of respect for Australian courts.
Sensing the
growing threat to its chance of holding onto government Messrs. Scott Morrison
and Peter Dutton are finally allowing very ill children detained in offshore
detention on Nauru to enter Australia for medical treatment.
ABC
News, 22
October 2018:
Australian Border Force
officials have revealed 11 children were transferred off Nauru today for
medical attention, with another 52 minors remaining on the Pacific island.
Officials have amended
the figure to 11 after initially saying it was 16.
The update comes as the
federal Greens float a compromise agreement that could allow families to
resettle in New Zealand with their families.
The Federal Government
has indicated it may accept New Zealand's offer to take up to 150
refugees, but only if legislation passes Parliament ensuring people sent to
offshore detention can never travel to Australia.
Home Affairs secretary
Michael Pezzullo said that legislation, which has been sitting in Federal
Parliament since 2016, would close a "back door" to dissuade further
boat arrivals.
According to the latest
figures, there are 652 people on Nauru, with 541 classed as refugees and 23 as
failed asylum seekers. The status of another 88 is yet to be determined.
The United States has
accepted 276 people as part of a resettlement deal and rejected an additional
148.
There is growing
pressure from crossbench MPs for the Government to accept New Zealand's offer,
with incoming independent Kerryn Phelps describing the issue as a first
priority.
The Greens are now open
to considering a travel ban for the group, but only if all children are first
brought to Australia for medical treatment, and restrictions only applied to
the cohort sent to New Zealand.
"We need to put the
politics aside and look after these children, who are being traumatised and
brutalised right now," leader Richard Di Natale told the ABC.
"If resettlement
after that means resettlement in New Zealand with limited restrictions, just on
that group, that's something we will consider.
"What we won't
consider is putting bans or restrictions [on] those people who have been left
behind.".....
Wednesday 29 August 2018
“Shit Life Syndrome” is sending Britons and Americans to an early grave…..
With Scott Morrison as the new prime minister, the Abbott-Turnbull era persistent attacks on the social fabric of the nation are bound to continue. Thus ensuring that Australians follow down the same path as Britain and America?
The
Guardian, 18
August 2018:
Britain
and America are in the midst of a barely reported public health crisis. They
are experiencing not merely a slowdown
in life expectancy, which in many other rich countries is continuing
to lengthen, but the start of an alarming increase in death rates across
all our populations, men and women alike. We are needlessly allowing our people
to die early.
In
Britain, life expectancy, which increased steadily for a century, slowed
dramatically between 2010 and 2016. The rate of increase dropped by 90% for
women and 76% for men, to 82.8 years and 79.1 years respectively. Now, death
rates among older people have so much increased over the last two years – with
expectations that this will continue – that two major insurance companies,
Aviva and Legal
and General, are releasing hundreds of millions of pounds they had been
holding as reserves to pay annuities to pay to shareholders instead. Society,
once again, affecting the citadels of high finance.
Trends
in the US are more serious and foretell what is likely to happen in Britain
without an urgent change in course. Death rates of people in
midlife (between 25 and 64) are increasing across the racial and ethnic
divide. It has long been known that the mortality rates of midlife American
black and Hispanic people have been worse than the non-Hispanic white
population, but last week the British Medical Journal
published an important study re-examining
the trends for all racial groups between 1999 and 2016.
The
malaises that have plagued the black population are extending to the
non-Hispanic, midlife white population. As the report states: “All cause
mortality increased… among non-Hispanic whites.” Why? “Drug overdoses were the
leading cause of increased mortality in midlife, but mortality also increased
for alcohol-related conditions, suicides and organ diseases involving multiple
body systems” (notably liver, heart diseases and cancers).
US
doctors coined a phrase for this condition: “shit-life syndrome”. Poor
working-age Americans of all races are locked in a cycle of poverty and
neglect, amid wider affluence. They are ill educated and ill trained. The jobs
available are drudge work paying the minimum wage, with minimal or no job
security. They are trapped in poor neighbourhoods where the prospect of owning
a home is a distant dream. There is little social housing, scant income support
and contingent access to healthcare.
Finding meaning in life is close to
impossible; the struggle to survive commands all intellectual and emotional
resources. Yet turn on the TV or visit a middle-class shopping mall and a very
different and unattainable world presents itself. Knowing that you are
valueless, you resort to drugs, antidepressants and booze. You eat junk food
and watch your ill-treated body balloon. It is not just poverty, but growing
relative poverty in an era of rising inequality, with all its psychological
side-effects,
that is the killer.
Shit-life
syndrome captures the truth that the bald medical statistics have economic and
social roots. Patients so depressed they are prescribed or seek opioids – or
resort to alcohol – are suffering not so much from their demons but from the
circumstances of their lives. They have a lot to be depressed about. They, and
tens of millions like them teetering on the edge of the same condition,
constitute Donald Trump’s electoral base, easily tempted by rhetoric that pins
the blame on dark foreigners, while castigating countries such as Finland or
Denmark, where the trends are so much better, as communist. In Britain, they
were heavily represented among the swing voters who delivered Brexit.
Read the full
article here.
NOTE: The last time the United States saw a prolonged life expectancy decrease due to natural causes was during the Spanish Influenza pandemic of 1917-1919 when life expectancy fell by twelve years.
Labels:
access & equity,
economics,
health,
inequality,
life expectancy,
society
Tuesday 7 August 2018
Australian Digital Health Agency is considering adding DNA data to My Health Record
Crikey.com.au, 6 April 2018:
DNA DEBATE
The federal government’s
controversial My Health Record program is capable of storing genomic data, such
as cancer risks, using technology that both has huge research applications and
highlights privacy and security concerns.
The Sydney Morning Herald reports that
genome-sequencing company Genome.One, which can track genetic variations and
therefore disease risks, has built “necessary infrastructure” for uploading
sensitive genomic data into the opt-out system.
University of Canberra privacy expert Bruce
Arnold has criticised the inherent risks of DNA-tracking technology and,
just a week after the government backdown on police access to My Health Records, today’s news as
again demonstrating a lack public consultation.
The Australian Digital Health Agency (ADHA) which is responsibe for My Health Record gave Genome.One, a wholly-owned subsidiary of The Garvan Institute, $40,000 in September 2017 to support the development of this software.
Its GoExplore™ software provides sequencing and analyses of patients’ DNA samples to assesses their risk of developing 52 hereditary conditions, including 31 cancers, 13 heart conditions, as well several other conditions where monitoring or intervention can be of benefit.
In a change of focus, Genome.One and The Garvan Institute are reportedly no longer offering clinical reporting for genetic disease diagnosis or personal health genomics in Australia. This service was priced at $6,400 plus GST, with no Medicare rebate.
Staffing numbers in Genome.One have been severely cut, new capital is being sought and, Gavan has
stated that it intends to spin off Genome.One
software into a new company in which it will be a minority shareholder.
However, Genome.One still intends to pilot its genomics technology integrated into GP practice software and on !8 April 2018 its CEO stated; “We're working with some electronic medical record providers and we're hoping that we can get a trial underway at some point this year”.
Labels:
Big Brother,
big data,
data retention,
genetics,
health,
information technology,
privacy,
safety
Thursday 2 August 2018
NSW Roads & Maritime Services finally come clean: We don't give a damn about any of the concerns Woombah & Iluka residents have about our asphalt plant, it's only Pacific Complete's bottom line that matters
ROADS and Martime
Services has revealed it will build at least two asphalt batching plants near
the Pacific Highway, most likely between Tyndale and the Iluka turnoff, next
year.
Pacific Highway general
manager Bob Higgins said the RMS has pressed the pause button on construction
of one plant at Woombah, but the need to supply the Glenugie to Iluka Rd
turnoff section with 170,000 tonnes of asphalt would require two plants.
He said the RMS would
review the supply strategy for the manufacture and delivery of asphalt on the
stretch of highway upgrade after protests from the Woombah community.
But Mr Higgins said if push came to shove when the RMS
review decided on locations, residents’ objections would take second place to
the technical needs of the project. [my yellow highlighting]
What a travesty Pacific Highway Upgrade community consultations are cannot get much clearer than this.
I'm sure local residents will not be pleased to have their fears confirmed.
I'm sure local residents will not be pleased to have their fears confirmed.
Whether he meant to or not, Bob Higgins
has probably just cemented the proposed Woombah asphalt batching site as a March 2019 NSW
state election issue in the Clarence electorate for both the NSW National
Party and the Berejiklian Coalition Government.
No-one likes to be told their valid concerns - about environmental impact, road safety, air quality and potential reduction in tourism numbers which underpin the local economy - don't matter to the state government down in Sydney.
BACKGROUND
No-one likes to be told their valid concerns - about environmental impact, road safety, air quality and potential reduction in tourism numbers which underpin the local economy - don't matter to the state government down in Sydney.
BACKGROUND
Labels:
#BerejiklianGovernmentFAIL,
environment,
health,
Iluka,
NSW Nationals,
Pacific Highway,
roads,
safety,
Woombah
Sunday 29 July 2018
When it comes to My Heath Record the words horse, stable, door, spring to mind
In January
2016 the Australian Digital Health
Agency (ADHA) became a corporate Commonwealth established under the Public Governance,
Performance and Accountability (Establishing the Australian Digital Health
Agency) Rule.
It has a
board appointed by the Minister for Health in whose portfolio it is situated and the board is the accountable
body of the ADHA.
Currently Mr Jim Birch AM, Chair. Mr Rob Bransby, Dr Eleanor Chew, Dr Elizabeth Deven, Ms Lyn McGrath, Ms Stephanie Newell, Dr Bennie Ng, Professor Johanna Westbrook and Michael Walsh sit on this board.
Currently Mr Jim Birch AM, Chair. Mr Rob Bransby, Dr Eleanor Chew, Dr Elizabeth Deven, Ms Lyn McGrath, Ms Stephanie Newell, Dr Bennie Ng, Professor Johanna Westbrook and Michael Walsh sit on this board.
The executive team is headed by Tim Kelsey as CEO, with Professor Meredith Makeham as Chief Medical Adviser and Bettina McMahon, Ronan O’Connor, Terrance Seymour & Dr. Monica Trujillo as the four executive managers.
ADHA is also
the designated Systems Operator for My
Health Record which currently
holds the personal health information of 5.98 million people across the country
and will add the remaining 19 million after 15 October 2018 unless they opt
out of being included in this national database.
Given the potential size of this database the question of cyber security springs to mind.
It seems that the Australian Digital Health Agency has not been independently audited for cyber resilience by the Australian National Audit Office (ANAO) ahead of beginning the mammoth task of collecting and collating the personal heath information of those19 million people.
Australian National Audit Office, Potential audit: 2018-19:
Management of cyber security risks in My Health Record
Australian National Audit Office, Potential audit: 2018-19:
Management of cyber security risks in My Health Record
The audit would examine the effectiveness of the Australian Digital Health Agency’s management of cyber security risks associated with the implementation and ongoing maintenance of the My Health Record system.
My Health Record creates a record of Australians’ interactions with healthcare providers, and more than 5.5 million Australians have a My Health Record. The audit would focus on whether adequate controls are in place to protect the privacy and integrity of individual records.It seems that the Australian general public still only has the honeypot's dubious word that it cannot be raided by unauthorised third parties.
Prime Minister Malcolm Turnbull has reacted to growing community concern about the number of agencies which can access My Health Records with a vague promise of "refinements" and with this outright lie; "The fact is that there have been no privacy complaints or breaches with My Health Record in six years and there are over 6 million people with My Health Records".
The Office of the Australian Information Commissioner has recorded complaints and at least 242 individual My Health Records have been part of mandatory data breach reports in 2015-16 to 2016-17, with nine of the 51 reported breach events involving "the unauthorised access of a healthcare recipient’s My Health Record by a third party".
BACKGROUND
Intermedium, 8 May 2018:
Re-platforming options
for the My Health Record (MHR) system will soon be up for consideration, with
an Australian Digital Health Agency (ADHA) spokesperson confirming that a
request for information will be released in the next few months to inform plans
to modernise the infrastructure underpinning Australia’s mammoth patient health
database.
An open-source,
cloud-based environment has already
been flagged as a possibility for the MHR by Department of Health
(DoH) Special Adviser for Strategic trategic Health Systems and Information Management Paul Madden at Senate Estimates in May last year. He also said that the re-platforming decision was one of many “variables” that needed to be squared away to accurately gauge how much the MHR system will cost beyond 2019-20.
“The variables in there include the re-platforming of the system to an open source environment, using cloud technology… which will be something we will not know the cost of until we hit the market to get a view on that”, Madden said last year. “Our commitment is to come back to the budget in 2019 to paint out those costs for the four years beyond.”
ADHA is scoping out MHR re-platforming options early, with the existing contract with the Accenture-led consortium not set to expire until 2020. As the “National Infrastructure Operator”, Accenture is tasked with running and maintaining MHR’s infrastructure. The prime contractor works with Oracle and Orion Health to provide the core systems and portals behind MHR.
Accenture was awarded the contract to design, build, integrate and test the then-personally controlled electronic health record system (PCEHR) back in 2011, and has signed 13 contracts worth a total of $709.53 million with DoH in relation to the MHR in that time. With the original infrastructure now over seven years old, ADHA recognise the importance of modernising the environment supporting the MHR....
What happens to medical
records when opting out?
Dr Kerryn Phelps reminds
us that, if people don't opt out, the My Health Records Act
allows disclosure of patients' health information to police, courts and the ATO
without a warrant ("My Health Record backlash builds",
July 25). This would be in addition to "health information such as
allergies, medicines and immunisations" available for emergency staff.
How can the access be
restricted to emergency staff? How can only certain categories of information
be released when allergies and medication are part of general medical notes? I
was not reassured by "serious penalties relating to the misuse of
information do not apply to accidental misuse" on the website. I opted
out.
My GP has told me that, nonetheless, she will be obliged
to upload my records
- which sounds credible since I have formally opted out with the government,
not with my doctor's practice. So what happens -
does my health record get kicked off "the cloud"?
What exactly did I opt out of?
Denise De Vreeze [my yellow highlighting]
Denise De Vreeze [my yellow highlighting]
Labels:
#TurnbullFAIL,
Big Brother,
data retention,
health,
information technology,
privacy,
safety
Tuesday 24 July 2018
Australian Health Minister Greg Hunt is not being truthful about My Health Record and he knows it
On 16 July 2018 the Australian Minister for Health and Liberal MP for Flinders, Gregory Andrew 'Greg' Hunt, characterised My Health Record as a "secure summary" of an individual's key health information.
The Office of the Australian Information Commissioner (OAIC) tells a rather different story.
One where at least 242 individual My Health Records have been part of mandatory data breach reports in 2015-16 to 2016-17, with nine of the 51 reported breach events involving "the unauthorised access of a healthcare
recipient’s My Health Record by a third party".
A story which also involves at least 96 instances of Medicare uploading data to the wrong digital health records and also uploading claim information to another 123 My Health Records apparently without the knowledge or consent of the persons in whose names these My Health Records had been created.
There were other instances where MyGov
accounts held by healthcare recipients were incorrectly linked to the My
Health Records of other healthcare recipients.
Prior to the database name change and system change from opt-in to opt-out there had been another 9 data breaches of an unspecified nature reported, involving an unknown number of what are now called My Health Records.
More instances are now being aired in mainstream and social media where My Health Records were created by DHS Medicare Repository Services or other agents/agencies without the knowledge or consent of the individual in whose name the record had been created.
Prior to the database name change and system change from opt-in to opt-out there had been another 9 data breaches of an unspecified nature reported, involving an unknown number of what are now called My Health Records.
More instances are now being aired in mainstream and social media where My Health Records were created by DHS Medicare Repository Services or other agents/agencies without the knowledge or consent of the individual in whose name the record had been created.
 |
| Healthcare IT News 16 July 2018 |
If this is how the national e-health database was officially functioning malfunctioning by 30 June 2017, how on earth is the system going to cope when it attempts to create millions of new My Health Records after 15 October 2018?
On the first day of the 60 day opt-out period about 20,000 people refused to have a My Health Record automatically created for them and at least one Liberal MP has also opted out, the Member for Goldstein and member of the House of Representatives Standing Committee on Health, Aged Care and Sport Tim Wilson.
Prime Minister Malcolm Bligh Turnbull has stated his view that mass withdrawals will not kill the national digital health records system - perhaps because he and his government are possibly contemplating adopting the following three coercive recommendations found amongst the thirty-one recommendations included in the Siggins Miller November 2016 Evaluation of the Participation Trials for the My Health Record: Final Report:
NOTES
OAIC annual reports:
On the first day of the 60 day opt-out period about 20,000 people refused to have a My Health Record automatically created for them and at least one Liberal MP has also opted out, the Member for Goldstein and member of the House of Representatives Standing Committee on Health, Aged Care and Sport Tim Wilson.
Prime Minister Malcolm Bligh Turnbull has stated his view that mass withdrawals will not kill the national digital health records system - perhaps because he and his government are possibly contemplating adopting the following three coercive recommendations found amongst the thirty-one recommendations included in the Siggins Miller November 2016 Evaluation of the Participation Trials for the My Health Record: Final Report:
20. Use all mechanisms
available in commissioning and funding health services as vehicles to require
the use of the My Health Record to obtain funds where practical.
21. Consider ways to
require the use of the My Health Record system by all healthcare providers and
how to best use the Government’s purchasing power directly (e.g. in the aged
care sector), via new initiatives as they arise (such the Health Care Home
initiative) or via PHNs commissioning clinical services (e.g. require use of
the My Health Record system in all clinical and aged care services that receive
Commonwealth funds). Such requirements should have a timeframe within which
healthcare providers need to become compliant.
22. Explore with health
insurers how they could encourage preferred suppliers and clients to use the My
Health Record system as part of their push for preventive care and cost
containment.
That the My Health Record is not about improving health service delivery for individual patients is indicated by the fact that a My Health Record is retained by the National Repositories Service for between 30 and up to 130 years after death and, even during an individual's lifetime can be accessed by the courts, police, other government agencies and private corporations listed as research organisations requiring medical/lifestyle information for what is essentially commercial gain, at the discretion of the Secretary of the Department of Health or the Digital Health Agency Systems Operator. See: My Health Records Act 2012 (20 September 2017), Subdivision B - s63 to s70
To put it bluntly, this national database will allow federal government to monitor the personal lives of Australian citizens more closely, enforce civil & criminal law, monetise collated data for its own benefit and, weaponize the personal information collected anytime it feels threatened by dissenting opinion.
NOTES
OAIC annual reports:
The Guardian, 22 July 2018:
Australia’s impending My
Health Record system is “identical” to a failed
system in England that was cancelled after it was found to be selling
patient data to drug and insurance companies, a British privacy expert has
said.
My Health Record is a
digital medical record that stores
medical data and shares it between medical providers. In the UK, a similar
system called care.data was announced in 2014, but cancelled in 2016 after an
investigation found that drug and insurance companies were able to buy
information on patients’ mental health conditions, diseases and smoking habits.
The man in charge of
implementing My Health Record
in Australia, Tim Kelsey, was also in charge of setting up care.data.
Phil Booth, the
coordinator of British privacy group Medconfidential, said the similarities
were “extraordinary” and he expected the same privacy breaches to occur.
“The parallels are
incredible,” he said. “It looks like it is repeating itself, almost like a
rewind or a replay. The context has changed but what is plainly obvious to us
from the other side of the planet, is that this system seems to be the 2018
replica of the 2014 care.data.” [my yellow highlighting]
North Coast
Voices , 22 July 2018, Former
Murdoch journalist in charge of MyHealth records –what could possibly go wrong?
UPDATE
Australian
Parliamentary Library, Flagpost,
23 July 2018:
Section 70 of the My Health Records Act
2012 enables the System Operator (ADHA) to ‘use or disclose
health information’ contained in an individual’s My Health Record if the ADHA
‘reasonably believes that the use or disclosure is reasonably necessary’ to,
among other things, prevent, detect, investigate or prosecute any criminal
offence, breaches of a law imposing a penalty or sanction or breaches of a
prescribed law; protect the public revenue; or prevent, detect, investigate or
remedy ‘seriously improper conduct’. Although ‘protection of the public
revenue’ is not explained, it is reasonable to assume that this might include
investigations into potential fraud and other financial offences involving
agencies such as Centrelink, Medicare, or the Australian Tax Office. The
general wording of section 70 is a fairly standard formulation common to
various legislation—such as the Telecommunications
Act 1997—which appears to provide broad access to a wide range of agencies
for a wide range of purposes.
While this should mean
that requests for data by police, Home Affairs and other authorities will be
individually assessed, and that any disclosure will be limited to the minimum
necessary to satisfy the request, it represents a significant reduction in the
legal threshold for the release of private medical information to law
enforcement. Currently, unless a patient consents to the release of their
medical records, or disclosure is required to meet a doctor’s mandatory
reporting obligations (e.g. in cases of suspected child sexual abuse), law
enforcement agencies can only access a person’s records (via their doctor) with
a warrant, subpoena or court order....
It seems unlikely that
this level of protection and obligation afforded to medical records by the
doctor-patient relationship will be maintained, or that a doctor’s judgement
will be accommodated, once a patient’s medical record is uploaded to My Health
Record and subject to section 70 of the My Health Records Act 2012. The
AMA’s Guide
to Medical Practitioners on the use of the Personally Controlled Electronic
Health Record System (from 2012) does not clarify the situation.
Although it has
been reported that
the ADHA’s ‘operating policy is to release information only where the request
is subject to judicial oversight’, the My Health Records Act 2012 does
not mandate this and it does not appear that the ADHA’s operating policy is
supported by any rule or regulation. As legislation would normally take
precedence over an agency’s ‘operating policy’, this means that unless the ADHA
has deemed a request unreasonable, it cannot routinely require a law
enforcement body to get a warrant, and its operating policy can be ignored or
changed at any time.
The Health
Minister’s assertions that no one’s data can be used to ‘criminalise’
them and that ‘the Digital Health Agency has again reaffirmed today that
material … can only be accessed with a court order’ seem at odds with the
legislation which only requires a reasonable belief that disclosure of a
person’s data is reasonably necessary to prevent, detect, investigate or
prosecute a criminal offence…..
Although the disclosure
provisions of different agencies may be more or less strict than those of the
ADHA and the My Health Records Act 2012, the problem with the MHR system
is the nature of the data itself. As the Law Council of Australia notes,
‘the information held on a healthcare recipient’s My Health Record is regarded
by many individuals as highly sensitive and intimate’. The National Association
of People with HIV Australia has
suggested that ‘the department needs to ensure that an individual’s My
Health Record is bound to similar privacy protections as existing laws relating
to the privacy of health records’. Arguably, therefore, an alternative to the
approach of the current scheme would be for medical records registered in the
MHR system to be legally protected from access by law enforcement agencies to
at least the same degree as records held by a doctor.
Subscribe to:
Posts (Atom)